Alzheimer’s disease remains one of the most pressing health concerns globally, given its devastating impacts on cognitive function, memory, and the quality of life. Among the various treatment options available, rivastigmine stands out, often touted for its potential benefits. This article delves into rivastigmine—its mechanism, benefits, side effects, and overall role in Alzheimer’s management—offering a critical lens on its efficacy and utility in real-world scenarios.
Understanding Alzheimer’s Disease and Its Impacts
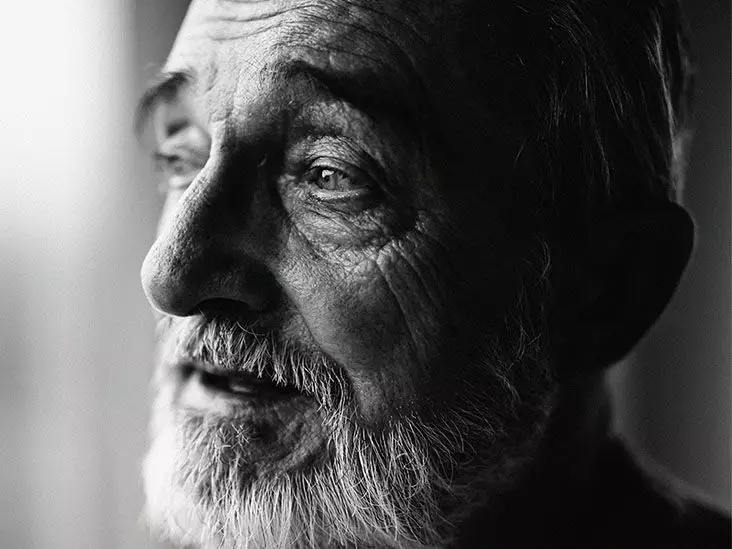
Alzheimer’s disease is not merely a memory disorder; it encompasses a cluster of cognitive impairments that progressively diminishes a person’s independence and fulfillment. It is prevalent in older populations and remains the leading cause of dementia. Unlike typical age-related cognitive decline, Alzheimer’s afflicts individuals with severe impairments in memory, thinking, conversation capability, and the execution of everyday tasks. Despite extensive research, Alzheimer’s remains incurable, and current treatments prioritize managing symptoms rather than reversing the disease’s trajectory.
Rivastigmine belongs to the class of cholinesterase inhibitors, which work to enhance acetylcholine levels in the brain—a neurotransmitter essential for memory and learning. In individuals with Alzheimer’s, the enzyme cholinesterase that breaks down acetylcholine is excessively active, leading to its depletion. By inhibiting this enzyme, rivastigmine prolongs the action of acetylcholine, theoretically improving cognitive function. The FDA approved rivastigmine in 1997, targeting patients experiencing mild to moderate stages of Alzheimer’s disease.
While the mechanism sounds promising, it’s crucial to recognize that enhanced acetylcholine alone does not suffice to counter the disease’s complexities. Emerging science suggests that merely increasing neurotransmitter levels may not translate to substantial cognitive gains or improvements in daily functioning, leaving room for skepticism regarding rivastigmine’s overall effectiveness.
Investigations into rivastigmine have yielded mixed results. Research indicates that patients using rivastigmine patches demonstrated better performance in cognitive testing than those on placebos. However, studies emphasizing rivastigmine’s benefits primarily address memory and daily activities, neglecting behavioral symptoms exacerbated by the disease. A significant limitation is that only a handful of studies documented observable changes in behavior, demonstrating that while some cognitive functions may improve, broader behavioral issues often necessitate more comprehensive interventions.
Furthermore, it’s important to critically consider the patch’s standout feature in delivering medication through the skin. While transdermal patches are innovative, they demand rigorous adherence to application protocols to maximize effectiveness. The instructions for applying and removing the patch may appear straightforward, yet inconsistent practices can compromise drug efficacy, making patient education paramount.
Potential Side Effects and Safety Concerns
Although rivastigmine is often perceived as a safer alternative to oral medications, it is not devoid of adverse effects. Common side effects encompass gastrointestinal disturbances, such as nausea and diarrhea, headaches, and dizziness. The possibility of more serious reactions, such as severe gastrointestinal bleeding or neurological events, raises legitimate concerns about the risk-to-benefit ratio of rivastigmine.
Prolonged monitoring by healthcare providers is advised in patients prescribed rivastigmine, as behavioral and physical side effects can arise or exacerbate over time. Moreover, the variability in patient responses underscores the need for personalized approaches in managing Alzheimer’s, highlighting that what works for one individual may not necessarily work for another.
Future Directions and Alternative Treatments
The limitations of rivastigmine and similar treatments illustrate the urgent need for innovative research in Alzheimer’s disease management. Alongside cholinesterase inhibitors, other classes of medications, such as NMDA antagonists (like memantine) and atypical antipsychotics, are emerging as alternative options to tackle various symptoms.
Yet, the implications of new treatments go beyond pharmacological interventions; they highlight the importance of comprehensive care, including non-pharmacological strategies like cognitive therapies, lifestyle modifications, and supportive care. As research progresses, a multifaceted approach may prove more effective in enhancing the overall well-being of individuals battling Alzheimer’s disease.
Rivastigmine continues to play a role in managing Alzheimer’s disease symptoms, but a critical assessment reveals its limitations. While it shows promise for improving certain aspects of cognitive function, rivastigmine does not alter the disease’s fundamental progression. As the medical community forges ahead in the quest for effective Alzheimer’s interventions, a balanced approach that combines medication with supportive therapies is crucial. Individuals considering rivastigmine should consult healthcare professionals to assess personal needs and evaluate the potential benefits and risks comprehensively.