Blood donation is a vital process that supports healthcare systems worldwide. Each donation is subject to rigorous testing protocols designed to ensure the safety and well-being of both the donor and the recipient. While routine tests are conducted for a range of conditions, leukemia is typically not included. This absence does not imply a lack of vigilance; rather, the nuances of blood testing are such that many abnormalities, including those related to serious conditions like leukemia, can still be identified through other means during the donation process.
Before any blood is collected, donors undergo a mini health assessment. This essential step includes checks for vital signs such as pulse, blood pressure, temperature, and crucially, hemoglobin levels, which indicate the presence of healthy red blood cells. Hemoglobin’s role is pivotal in transporting oxygen throughout the body, and abnormalities can signal underlying health issues, such as anemia or potentially leukemia. If any red flag arises during this initial evaluation, the healthcare professional will typically disqualify the donor from proceeding with the donation, prioritizing health over the immediate need for blood.
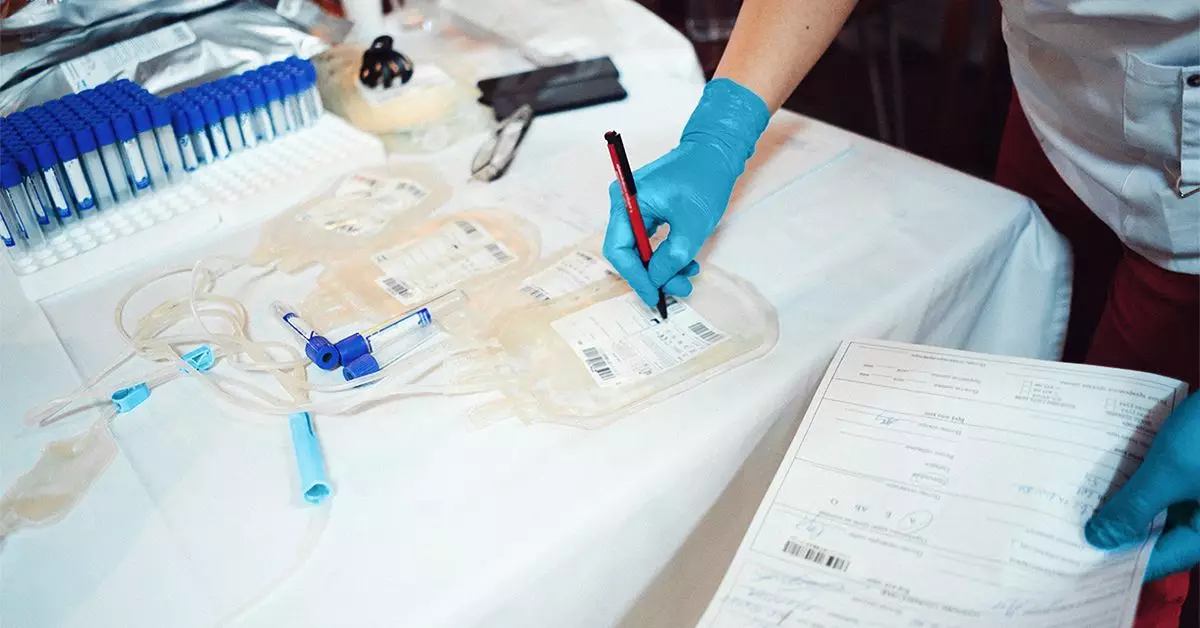
In addition to scouting for leukemia, blood donations are screened for various infectious diseases, a practice deemed critical for the safety of the blood supply. Organizations like the American Red Cross perform comprehensive analyses on each donation to identify blood type, sickle cell traits, and markers for infectious diseases. This might include tests for viruses such as HIV or Hepatitis, ensuring that every unit of blood is free from potentially harmful pathogens. Such screening is essential not only for recipient safety but also helps protect the ongoing integrity of the blood donation framework.
One intriguing aspect of blood donation and its associated testing is the small risk linked to the HTLV-1 virus, which can, in rare instances, lead to adult T-cell leukemia (ATL). This connection underlines the importance of routine screening; should a potential risk factor be identified in a donor, the blood is immediately discarded, and the donor is notified. Such follow-up action emphasizes the interconnectedness of health monitoring and blood donation.
Follow-Up and Healthcare Support
In scenarios where abnormalities are noted during the donation process, blood donation centers are proactive in their approach. Healthcare professionals may reach out to affected individuals, suggesting that they seek further medical advice. This follow-up not only emphasizes the organization’s commitment to donor well-being but also reinforces the healthcare system’s role in managing potential health concerns.
In sum, while testing for leukemia specifically may not be a standard component of blood donation procedures, the multifaceted approach to health assessment and blood screening plays a crucial role. Donors are intricately woven into a system designed to safeguard both their health and that of the blood recipients, ensuring that the blood donation process remains a safe and effective vital resource for society at large.